ADHD and pleasure-seeking systems
By Sophia DiLavore and Jim Stellar
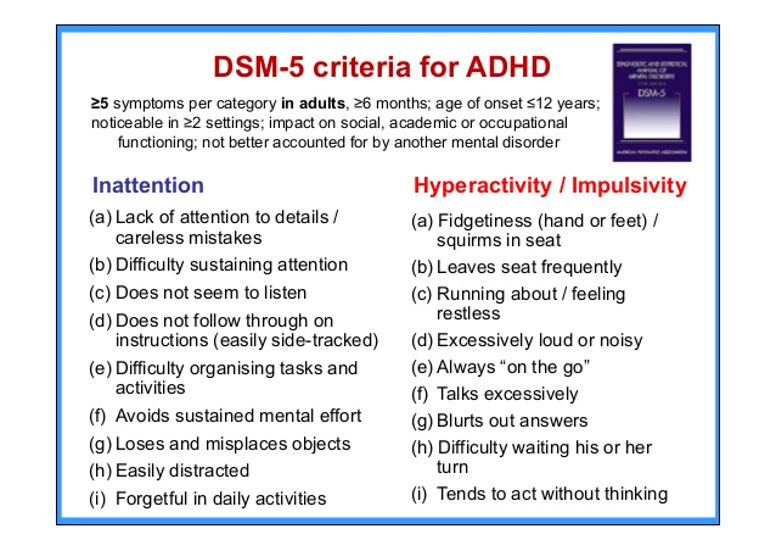
This blog is about the established idea that dopamine in the limbic system is important to Attention Deficit and Hyperactivity Disorder (ADHD) as defined by DSM5-TR and as shown in the figure below.
Following the history of this blog series, we also suggest that implicit learning in a college student’s internships complements the explicit learning from college courses to guide student career development in and after college. These two things are related and so the study of ADHD from this perspective could reveal aspects of cognitive-emotional integration in college students with and without ADHD.
First, we explore here the idea that in ADHD, the brain seeks pleasure in order to counteract the “fear” response deriving from uncomfortable situations where the ADHD patient cannot perform as well as they want. Second, we explore the idea that the ADHD brain seeks focus because that is the way to accomplish tasks, thus reducing the fear mentioned above, and of course gain pleasure. Both of these properties operate through the dopamine systems.
Let’s first discuss how pleasure-seeking works via dopamine and how that reduces fear in ADHD patients.
ADHD, dopamine, pleasure seeking, and focus
Dopamine (DA) is a neurotransmitter that has a long-held reputation for being involved in reward just as it has for being involved with Parkinson’s Disease and schizophrenia. In reward, dopamine comes from the ventral tegmental area (VTA) in the back of the midbrain and projects forward to the Nucleus Accumbens (NAc) in the front of the midbrain. Both of these structures are considered to be part of the limbic system, which somehow connects to the cognitive brain in the neocortex.
Rewards, stimuli that cause pleasant emotions, lead to behaviors that maximize pleasure and minimize pain/discomfort. We will return to this concept later. For now, one of the abnormalities of the ADHD brain is that it lacks a sufficient amount of DA receptor sites, which diminishes the impact of any DA that is released in reward centers like the NAc. This lack of dopaminergic activity postsynaptically drives a person with ADHD to engage in activities that will release DA production to overcome loss of DA receptor activation. For example, people with ADHD jump into action without thinking of the consequences which could explain why (especially children/adolescents) have difficulty following instructions, routines, and exhibit age inappropriate behavior compared to their peers. This trait is a reflection of an executive function deficit that we also discuss later.
To go into a bit more detail on DA receptors, there are believed to be 5 different types of receptors that are themselves coupled with intracellular G-proteins to mediate direct effects on neuron firing and to mediate internal biochemical effects that indirectly change cell firing. This complexity at the neuron level then gets translated into a brain circuit level that can affect behavior. The complexity of this system is why neuroscientists and clinicians are still studying ADHD. But we can already see the importance here because DA can have different functions through the different types of receptors and so can the drugs used to treat ADHD. Here we will discuss what is known about these mechanisms and how dopamine has a role not only in reward but also in memory, motivation, and learning – all of which are relevant to ADHD.
Dopamine receptor deficits in the reward pathway are apparent in ADHD subjects and are seen on a PET scan. They could have a variety of effects including facilitating a failure to delay gratification, i.e. impulsivity. We wrote about this phenomenon in a previous blog that also linked amygdala activation to the generation of fear ADHD subjects. One idea here is that a person with ADHD potentially prefers small immediate rewards instead of larger delayed rewards. In other words, a person with ADHD will have a stronger aversion towards delayed rewards which brings on a demotivating effect for hypothetical rewards. This concept promotes impulsivity when making choices. Also, insufficient amounts of chronic dopamine and abnormalities in the dopamine reward pathways can also explain attention deficits through this mechanism because tasks that are considered boring or unrewarding to a person with ADHD do not stimulate enough dopamine to draw focus. In other words, a proper dopamine-based reward system = sustained focus and ADHD patients may lack that DA release for long enough to sustain that focus.
ADHD and fear
Again as discussed in the previous blog, the amygdala is associated with emotional processing including fear. However, it is also known to be involved in performing some appetitive tasks for reward. Conditioned stimuli (CS) are processed within the basolateral amygdala (BLA) which can produce goal oriented and reward seeking behavior. These behaviors can be categorized as instrumental behavior, where voluntary actions are performed to achieve a specific outcome, and as consummatory behavior, which involves the actual consumption or enjoyment of the reward. The amygdala is activated during motivated behaviors as it stores conditioned and unconditioned stimulus memories within the corticostriatal circuit. These regions facilitate the integration of emotional and motivational processes, enabling one to pursue and achieve goals. The amygdala’s role in this network shows its significance in both emotional responses and survival driven behaviors that are necessary for environmental adaptation.
Because the BLA is required for appetitive and aversive reinforcement, the presence of lesions in this area can prevent conditioned stimuli from appropriately influencing an individual’s reaction. The BLA is necessary for Pavlovian CS but not for generalized CS-US associations. Specific Pavlovian-instrumental transfer “is the process by which a CS associated with a specific appetitive reinforcer can enhance instrumental responding for the same enforcer.” Instrumental behavior, actions executed to reach a goal, is influenced by the BLAs association between specific CS and US. The learned response of active avoidance by which an instrumental response is executed to avoid a negative outcome (negative reinforcement) is dependent on the BLA.
So what is the role of the BLA in processing appetitive and aversive stimuli? As discussed in the references above, the BLA acts as part of a memory storage device for CS-US pairings. In this thinking, BLA neurons encode associations between sensory cues and their emotional outcomes. During motivated behaviors (like eating or drinking) the BLA is activated processing the cues with emotional outcomes. Through a process known as value coding, the neurons within the BLA respond preferentially to rewarding or aversive cues when an individual exhibits approach or avoidance behaviors. The encoding of appetitive and aversive stimuli are also similar in that they share such qualities as salience and motivational significance. Thus the neurons in the BLA can respond to both types of stimuli. Finally, it is difficult to make an absolute distinction between appetitive and aversive stimuli properties because some types may also have mixed valence. So even though one may be able to distinguish different cues, there is a possible overlap in neuronal activity. The BLA processes emotional valence of stimuli (fear and reward) and factors related to safety and positive outcome prediction.
Dopamine and reward from pain/fear reduction
The nucleus accumbens (NAc) itself is most often associated with pleasure, reward, and addiction, but it also functions as a pain reduction mediator. This phenomenon is called dissociative analgesia and it comes about when the limbic system is biased by reward and NAc dopamine activation so that it does not allow pain to shape the behavior. The NA is obviously important for motivational behaviors that drive a person towards pleasure and away from pain. However, the NA does not work alone, as it connects with the prefrontal cortex, limbic system, and other brain regions. Its connections via feedback loops with brain areas involved in sensation, emotion, and cognition can show that the reward pathway is involved in relieving pain, not just seeking pleasure. This arrangement begs the question of whether the NAc actually manages physical pain. The existence of pain is necessary for survival instincts. It is critical in learning from past experiences that caused pain so that in the future similar experiences can be avoided. Endorphins are released in situations where it would be helpful to suppress pain in order to gain a reward. The analysis and classification of pain must occur so that motivational behaviors in the presence of pain can be appropriate.
ADHD, focus, and attention
People with ADHD classically have problems with focus and with attention.
Focus: A study with rats monitored dopamine levels in the NAc while the rats underwent a classical conditioning process. In the beginning of the experiment, rats’ dopamine levels spiked when they received the reward, but not before when there were cues that allowed them to potentially predict the reward. As the experiment continued, the rats learned and began associating the cues with rewards which caused the DA levels in the NA to spike when the cues were presented. This showed that the rats expected the reward before they received it. Only rats that were classically conditioned experienced this shift in dopamine release which confirms that they learned and responded to their experiences. The experiment shows that the release of dopamine is a kind of signal in the brain for anticipated rewards which are influenced by learned associations. In other words, dopamine allows us to predict rewards and motivates us to pursue them.
The dopaminergic firing rate to cues is different in the ADHD brain compared to the average non-ADHD brain. Similar to the experiment mentioned in the paragraph just above, children without ADHD have a dopaminergic response with the reward, but after repeated pairings with an anticipatory stimulus the DA response occurs with the stimulus instead. In the ADHD brain, the main difference lies in the shift of the dopaminergic response from the anticipatory stimulus to the reward. Less phasic dopamine is released during anticipation of reward cues in the ventral striatum. This reduced response leads to weaker conditioning, quicker behavior extinction, and weaker influence of reinforcement on behavior.
Attention (Signal to noise ratio) Dopamine deficits lower the signal to noise ratio making it difficult for the ADHD person to distinguish the signal from background noise. This could explain why during conversations or during active thought the ADHD person will struggle to follow along and become easily side tracked. All external sounds/conversations and thoughts are equally loud making it difficult to remain focused on a single continuous stream. They instead are drawn to several different stimuli from conversation or thought. Ample levels of dopamine in the ADHD brain whether it be from medication or intrinsic motivation amplifies the signal and drowns out the background noise allowing the ADHD person to follow along with the one signal/conversation.
ADHD, dopamine, and executive function
Finally, ADHD patients have executive dysfunction, which refers to cognitive abilities that are required to complete goals and involve memory, attention, and self regulation. The figure below illustrates some of the ways executive function interacts with ADHD.
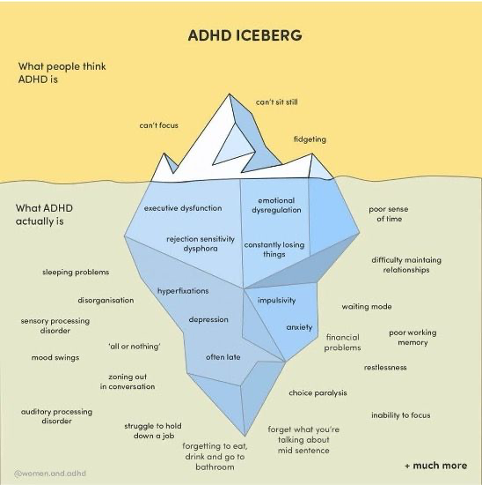
The DSM-5 diagnostic criteria for ADHD list several symptoms that coincide with executive functioning deficits. As stated in our previous blog the prefrontal cortex, the brain area heavily involved in executive functioning, in patients with ADHD is 3-5% smaller than the average. Executive functioning is required to successfully complete daily tasks which can be difficult when working memory, cognitive flexibility, and inhibition control are not working properly. Higher level executive functions like planning, reasoning, and problem solving are dependent on the functions listed above. One of the main struggles faced is self motivation. People with ADHD lack inhibition control which ultimately regulates emotions, thoughts, and actions. As discussed, learned behavior and motivational behavior allow one to respond situationally appropriately.
Decreased availability of the D2 and D3 receptors within the dopamine reward pathway directly cause hyperactive, impulsive, and delayed initiation of movements. In a study with rats, the deletion of the DRD2 polymorphism caused an extreme increase in reward behavior and hyperactivity which exemplifies the role of D2. Of course, rats are not quite humans genetically.
Consider the case of a college student who has 3 homework assignments and an exam that needs to be completed in 5 days. The ADHD student is fully aware that he must complete them, but cannot bring himself to start. He may procrastinate and wait until the last minute until he feels motivated by the deadline even though he will not complete the tasks to the best of his ability. If and when he manages to begin, he will be distracted by his thoughts or external environment. He will also have an inaccurate perception of time which leads him without enough time to complete tasks.
The student is also forgetful. Even though the student knew about the assignments over a week before, he forgot about them because he is disorganized. This scenario is representative of each day of an ADHD person. An exception to this is when the ADHD person finds an activity that stimulates interest in which case he is intrinsically motivated to act with ease.
Stimulant medications like ritalin (methylphenidate) are used to treat ADHD improving attention, focus, and executive function. Methylphenidate works specifically by inhibiting the reuptake of the neurotransmitters dopamine and norepinephrine. This prevents neurotransmitters from being reabsorbed into neurons within the brain. By doing this, neurotransmitter levels are increased in the synaptic cleft which enhances the signaling between neurons prolonging their action. Previously, it was thought that stimulants had a paradoxical effect for ADHD treatment because it was perceived as giving someone with hyperactivity more energy. However, recent studies have proven that stimulants are interacting with a chemical imbalance contributing to an underaroused brain. Due to low arousal, a person with ADHD constantly seeks stimulation from the environment to initiate neural activity. From a third person perspective this may be viewed as hyperactivity or inattention when in reality the ADHD person is unconsciously seeking dopamine.
We touched briefly on people with ADHD preferring smaller immediate rewards over larger delayed rewards above. To expand on this here, the catecholamines dopamine and norepinephrine that regulate attention and behavior in the PFC are released according to arousal state. When too little is released it results in boredom and when too much is released it induces a stress response. When optimal amounts are released the person with ADHD will be alert and interested in whatever he is doing. People with ADHD need constant reminders due to working memory problems and are unable to change their behaviors or plans to accommodate environmental demands. They tend to live in the moment and do not adapt to changes swiftly. The ADHD person knows they have tasks to complete but cannot bring themselves to begin.
The brain regulates the release of dopamine with phasic and tonic release mechanisms. Tonic firing occurs during baseline environmental conditions when there is a lack of unexpected stimuli whereas phasic release occurs when events of motivational significance (like unexpected rewards) are perceived. Both kinds of dopamine levels affect each other. For example, if an individual has a large amount of tonic dopamine then it can cause the phasic response to be smaller. People with ADHD have lower tonic levels causing their phasic responses to be bigger. Because there is less dopamine at baseline, greater stimulation is required to maintain sufficient levels. This concept can be observed in behavior of an ADHD person as the individual is hypersensitive to the environment. The person may be in the middle of speaking, working, writing, etc. and he immediately stops the task to explore something else he noticed whether it be a thought or a bird he just saw outside the window. This is why stimulant medications are effective treatments for ADHD. They target dopamine causing the ADHD brain to mimic the functioning of the average brain. After taking methylphenidate, the ADHD person’s arousal increases as there is more tonic dopamine lessening the phasic response. Then in turn the ADHD person feels less inclined to seek out more stimulation from the environment and finds it much easier to maintain focus.
ADHD gets better (changes) in the Adult
ADHD symptoms do not typically intensify with age; they may actually decline. As a person with ADHD matures, his symptoms may improve but the structural abnormalities remain. Until the 1990s ADHD was categorized as a childhood disorder but it is now recognized as being able to persist into adulthood. Specifically it is classified now as a neurodevelopmental disorder. Medication usage in children for ADHD grew 28% from 2007-2011. At the end of 2011 70% of children with ADHD used medication contrasting with only 11% of adults with ADHD taking the medication.
If ADHD doesn’t necessarily “get better” in the adult, the symptoms may change in their presentation. Three main types of ADHD are: predominantly hyperactive, predominantly inattentive, combined hyperactivity and inattention. Clinicians know that symptoms of hyperactivity tend to improve with age, usually decreasing in early adolescence; however they may be replaced with symptoms like restlessness in adulthood. It should be noted that hyperactive symptoms in adults could be viewed as less problematic because adults developed adaptive strategies to cope with their hyperactive symptoms. Impulsive behaviors may also improve with age, but it still exists with greater consequences due to the existence and availability of higher risk activities engaged in during adulthood. For example, the inattention symptoms tend to remain stable across age groups, but it could appear to worsen in adults because of the weight of adult daily activities like assignments in the workplace. Adults who were diagnosed in their childhood years tend to present more coping skills in adulthood, but this does not mean their ADHD has gone away. Children with undiagnosed ADHD could present an increased risk of other mental conditions and difficulty in adulthood.
Gender differences in ADHD
It is clear that boys are diagnosed more often than girls in childhood, but ADHD is not more common in boys, rather this disparity is due to the underdiagnosis of females due to differences in symptom presentation. Generally males with ADHD have visible symptoms and behaviors that are disruptive which explains why they are noticed more. Females are typically less disruptive and do not display obvious signs. Some key differences between females and males that make it difficult to recognize and diagnose girls are that females tend to show inattentive symptoms, they often develop adaptive behaviors that mask their symptoms, they present internally, they’re often misdiagnosed with a different disorder, their inattentive symptoms are noticed when they are in highschool when there is a more structured learning environment. Even when females do present similar behaviors as males with ADHD they may be missed or overlooked as a personality trait.
Neuroplasticity
Neuroplasticity could underlie some of these changes. For example, consider a mouse model of ADHD based on early nicotine administration. The ADHD behaviors seen in these mice were normalized in adult mice by MPH administration. In this mouse model neurobiological indicators were also normalized which suggests the kind of changes that might be going on with human aging. While such studies can not be done in humans, they generate hope that a better understanding of drug effects in the brain could lead to therapeutic outcomes. However, note that the preceding paragraph on gender differences reminds us that unlike laboratory mice, humans vary in many ways besides gender, and these differences would have to be taken into account if we were to try to use a drug to normalize a human ADHD brain. More encouragement comes from a recent study done in humans that found MPH stimulant effects improved ADHD symptoms and some brain structural abnormalities, particularly in reward-related brain areas. Of course, more research needs to be conducted to identify the long term effects of stimulants and we may return to discuss neuroplasticity again in another blog.
Summary
In summary, how does the ending of this blog relate to the opening idea that ADHD patients use reward to offset the fear of making a mistake due to the presence of their ADHD? The answer is that we do not know, but it certainly is intriguing and we may be back with more thinking on this topic. We do see the basic cognitive-emotional integration in ADHD as applying to everyone, even non-ADHD college students making decisions.
